Cancer care has advanced dramatically in recent years, with new diagnostic and therapeutic tools and treatments that are saving lives like never before. Yet as a new report shows, these advances are also costly, and access to the best therapies is far from assured to all.
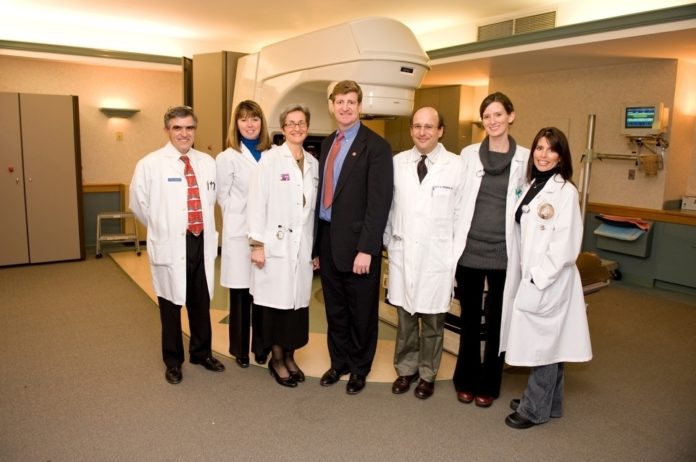
In December, NorthMain Radiation Oncology, a doctor-owned outpatient treatment center in Providence, invited Congressman Patrick J. Kennedy to visit and learn about the latest in radiation oncology – a particularly fast-changing field – and new challenges that are arising.
Dr. Scott A. Triedman, an oncologist at NorthMain and a clinical assistant professor at The Warren Alpert Medical School of Brown University, offered his perspective.
PBN: How widely is radiation used in oncology these days?
TRIEDMAN: About half of patients who develop cancer will receive radiation therapy as part of their treatment. It can be administered before surgery, after surgery or with no planned surgery. Radiation is also combined with chemotherapy for certain cancers. Pre-operative radiation is often given to shrink a tumor with the hope that it might make the surgery easier to successfully perform. Post-operative radiation is often given to kill any microscopic cancer that may persist after surgery. Radiation without surgery is sometimes used to try to both cure the cancer and to try and preserve critical organs. Sites where radiation alone may be considered include certain head and neck cancers, lung cancers, prostate cancers and lymphomas. Optimal treatment is determined through a multidisciplinary team approach that includes a surgeon, a medical oncologist and a radiation oncologist.
PBN: Radiation oncology has advanced and diversified a lot in recent years. What kinds of treatments do you offer?
TRIEDMAN: Radiation has been used to treat cancer for more than 100 years … [but] in the last 10 years there have been a number of significant technological advances that have radically improved both radiation treatment planning and delivery. Some of the most notable improvements include image-guided radiation therapy (IGRT), intensity modulated radiation therapy (IMRT), and high dose rate or (HDR) brachytherapy. At NorthMain Radiation Oncology, we have been on the leading edge of cancer treatment since our inception in 1978, and we offer each of those modalities.
IGRT is guided by imaging equipment such as CT, ultrasound or stereoscopic X-rays. Images are taken in the treatment room just before the patient is treated, allowing radiation to be delivered to tumors with more precision and with less normal tissue irradiated.
IMRT has been a major advance over traditional 3-D conformal radiation in which two to six individually shaped beams were used to treat the tumor. IMRT is a type of external beam radiation in which hundreds of individually shaped “beamlets” of radiation are delivered from many different angles to the target area. …
HDR brachytherapy utilizes radioactive materials that are placed temporarily in body tissue or cavities. These treatments usually last a few minutes, and then the radioactive source is removed. We are using HDR for accelerated partial breast irradiation, certain gynecologic malignancies and some skin cancers. HDR shortens the treatment course for eligible breast cancer patients from seven weeks down to one week.
PBN: Patients have a choice between independent facilities like yours and hospital settings. What are the pros and cons of being treated at a place like NorthMain instead of a hospital?
TRIEDMAN: The one thing that clearly sets us apart is our focus on being “patient-friendly.” We go out of our way to make the often lengthy and difficult treatment process as easy on the patient and their families as possible. We also pay attention to all the small details that often mean a lot to the patient, such as scheduling of treatments, convenience of location and providing in-house counseling and support services. At the same time, we provide the same latest technologies, experienced board-certified physicians and access to clinical trials that are available in a large medical center.
PBN: All this equipment is extremely expensive, and insurers’ reimbursement rates have tended to reflect that. In an era of high-deductible plans and growing uninsurance, are you seeing more patients struggle to cover the cost of their treatment? Are insurers also pushing back in trying to control the cost of your services?
TRIEDMAN: Unfortunately, we are all seeing increasing numbers of uninsured or underinsured patients in our practice. This certainly compounds the tremendous stress that our cancer patients endure. We treat all patients regardless of their ability to pay. In addition, from a health care provider perspective, many of our fixed costs have continued to increase, and our new technology and staffing costs remain substantial. The insurers continue to control and often reduce reimbursement for radiation services.
PBN: You were recently visited by Congressman Patrick Kennedy. Can you tell us about that visit, and the topics you discussed?
TRIEDMAN: We were honored to have Congressman Kennedy at our facility. At that visit we discussed the clinical and economic challenges that lie ahead in the fight against cancer. Our primary goal was to show him just how effective cancer care can be when you combine clinical excellence with compassionate care. We also discussed the important role that free-standing radiation oncology centers play in what is primarily an outpatient therapy. In addition, we discussed the many new and exciting technologies that we now have available.
PBN: How widely is radiation used in oncology these days?
TRIEDMAN: About half of patients who develop cancer will receive radiation therapy as part of their treatment. It can be administered before surgery, after surgery or with no planned surgery. Radiation is also combined with chemotherapy for certain cancers. Pre-operative radiation is often given to shrink a tumor with the hope that it might make the surgery easier to successfully perform. Post-operative radiation is often given to kill any microscopic cancer that may persist after surgery. Radiation without surgery is sometimes used to try to both cure the cancer and to try and preserve critical organs. Sites where radiation alone may be considered include certain head and neck cancers, lung cancers, prostate cancers and lymphomas. Optimal treatment is determined through a multidisciplinary team approach that includes a surgeon, a medical oncologist and a radiation oncologist.
PBN: Radiation oncology has advanced and diversified a lot in recent years. What kinds of treatments do you offer?
TRIEDMAN: Radiation has been used to treat cancer for more than 100 years … [but] in the last 10 years there have been a number of significant technological advances that have radically improved both radiation treatment planning and delivery. Some of the most notable improvements include image-guided radiation therapy (IGRT), intensity modulated radiation therapy (IMRT), and high dose rate or (HDR) brachytherapy. At NorthMain Radiation Oncology, we have been on the leading edge of cancer treatment since our inception in 1978, and we offer each of those modalities.
IGRT is guided by imaging equipment such as CT, ultrasound or stereoscopic X-rays. Images are taken in the treatment room just before the patient is treated, allowing radiation to be delivered to tumors with more precision and with less normal tissue irradiated.
IMRT has been a major advance over traditional 3-D conformal radiation in which two to six individually shaped beams were used to treat the tumor. IMRT is a type of external beam radiation in which hundreds of individually shaped “beamlets” of radiation are delivered from many different angles to the target area. …
HDR brachytherapy utilizes radioactive materials that are placed temporarily in body tissue or cavities. These treatments usually last a few minutes, and then the radioactive source is removed. We are using HDR for accelerated partial breast irradiation, certain gynecologic malignancies and some skin cancers. HDR shortens the treatment course for eligible breast cancer patients from seven weeks down to one week.
PBN: Patients have a choice between independent facilities like yours and hospital settings. What are the pros and cons of being treated at a place like NorthMain instead of a hospital?
TRIEDMAN: The one thing that clearly sets us apart is our focus on being “patient-friendly.” We go out of our way to make the often lengthy and difficult treatment process as easy on the patient and their families as possible. We also pay attention to all the small details that often mean a lot to the patient, such as scheduling of treatments, convenience of location and providing in-house counseling and support services. At the same time, we provide the same latest technologies, experienced board-certified physicians and access to clinical trials that are available in a large medical center.
PBN: All this equipment is extremely expensive, and insurers’ reimbursement rates have tended to reflect that. In an era of high-deductible plans and growing uninsurance, are you seeing more patients struggle to cover the cost of their treatment? Are insurers also pushing back in trying to control the cost of your services?
TRIEDMAN: Unfortunately, we are all seeing increasing numbers of uninsured or underinsured patients in our practice. This certainly compounds the tremendous stress that our cancer patients endure. We treat all patients regardless of their ability to pay. In addition, from a health care provider perspective, many of our fixed costs have continued to increase, and our new technology and staffing costs remain substantial. The insurers continue to control and often reduce reimbursement for radiation services.
PBN: You were recently visited by Congressman Patrick Kennedy. Can you tell us about that visit, and the topics you discussed?
TRIEDMAN: We were honored to have Congressman Kennedy at our facility. At that visit we discussed the clinical and economic challenges that lie ahead in the fight against cancer. Our primary goal was to show him just how effective cancer care can be when you combine clinical excellence with compassionate care. We also discussed the important role that free-standing radiation oncology centers play in what is primarily an outpatient therapy. In addition, we discussed the many new and exciting technologies that we now have available.










