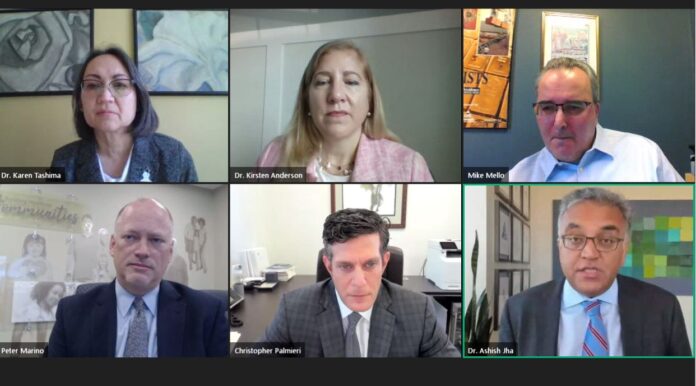
PROVIDENCE — Rhode Island has improved its vaccination campaign to a point where it is among the nation’s most successful in administering first doses, but the effort to reach people who are reluctant to be vaccinated remains a significant challenge in fully controlling the pandemic, according to panelists at PBN’s Health Care Summit on Thursday.
After a sluggish start, the state has picked up speed in the last four to six weeks, although variants that are more contagious and may cause more serious illness and death remain a concern, the panelists said.
Very soon, however, so-called vaccine hesitancy will become the larger issue for the state, according to Dr. Ashish Jha, dean of the School of Public Health at Brown University.
“The real challenge, the real policy challenge, social challenge, is what happens once we get into May,” Jha said during one of two panel discussions during the virtual summit Thursday. “We’re going to have a chunk of Rhode Islanders who are unvaccinated, and we will have plenty of vaccines. And we will have to work really hard on issues of hesitancy, on issues of access, making sure we’re engaging trusted voices to become advocates for vaccinations.”
Several panelists agreed that the increasing rate of vaccinations will help to blunt spikes in infection that may happen over the next several months. Rhode Island, like many other states, is now seeing an increasing share of the B.1.1.7, or U.K. variant, which is far more infectious than the original strain that hit last year. Data also suggests it is more deadly, according to Jha.
Because the available vaccines are now only available to people who are 16 and older, this means children cannot be vaccinated at this point. Until 80% to 90% of the community is vaccinated to reach so-called “herd immunity,” the state will continue to see outbreaks, Jha estimated.
Dr. Karen Tashima, who directs clinical trials for Lifespan Corp. and who was the principal investigator for two Remdesivir studies in Rhode Island for moderate and severe COVID-19 cases, said she is concerned that computer-based appointments for vaccine remain an obstacle for many people who lack access to technology.
“There has been a good effort in Rhode Island to get to ZIP codes and areas of the city where access would be predicted to be lower. But we’re still not where we need to be in those areas,” she said.
Making appointments remains largely a technology-driven task, she said. “It’s been a challenge … having to go online and so many of my patients don’t have the capability of doing that.”
Primary care offices that are making calls directly to patients and encouraging them to visit local vaccine clinics is worthwhile, she said. “For a lot of people, it has not been that easy and it’s not just the older folks who are having trouble with that.”
Christopher Palmieri, CEO and president of Commonwealth Care Alliance, said his company has made a priority of reaching people who are homebound and cannot get to vaccine appointments. The company is trying to reach 25,000 people in Massachusetts who are homebound.
Panelists also addressed some of the business implications of the continuing pandemic, including whether companies should be requiring employees to receive vaccinations and whether people can start to end precautions such as wearing masks once herd immunity is reached.
Dr. Kirsten Anderson, who is the senior director of clinical solutions for New England for Aetna/CVS Health, said if universities can help make access to the vaccine easier for young adults by making those vaccines available on-campus.
Palmieri said with 1,500 employees, many of them front-line health workers, CCA has a high vaccination rate. “We are not in the conversation now as to whether we require it. We want to make sure it is available.”
Peter Marino, CEO of Neighborhood Health Plan of Rhode Island, said requiring vaccinations for its 600 employees also has not been its approach. “I do think businesses have the legal authority to mandate vaccines, the real question is should they mandate vaccines. In Neighborhood Health’s case, we are not there.”
Another panel of health care industry leaders discussed what steps Rhode Island can take towards health equity, increased affordability for services and use of telemedicine.
The panelists included R.I. Health Insurance Commissioner Patrick Tigue; Dr. Michael Bradley, president and CEO of Ortho Rhode Island; Dr. Claire Levesque, Tufts Health Plan chief medical officer for commercial products; and Dr. Matt Collins, chief medical officer and executive vice president of Blue Cross & Blue Shield of Rhode Island.
Tigue said the priorities of increasing affordability should be to move to value-based payments plans rather than fee-for-service plans, focus on community investments outside of health to ensure that initiatives such as housing and transportation are sufficiently prioritized and to take action on decreasing prescription drug prices. With a drop in volume of many health services during the pandemic, medical providers suffered financially; having a system that incentivizes quality and serving patients well, he said, will both help health care companies financially and assist public health.
Access to other vaccines was something Levesque discussed. She noted Tufts gave a $50 incentive to parents who brought their children to a pediatrician for a flu vaccine. “We did that because we wanted to get them back into the pediatrician and to get all their catchup vaccines,” she said. “So people were not getting their children in for the measles vaccine. We don’t want to follow up a COVID pandemic with a measles pandemic.”
Also discussed was an initial decision by Blue Cross & Blue Shield to no longer waive cost-share or out-of-pocket treatment for COVID-19 as of April 1. That decision was later reversed, and Collins said the initial decision came as a result of forecasts about the spread of the virus. “We picked March 31, and we would revert to what the original plan was, which was some out-of-pocket cost-sharing,” he said. When the insurer contacted customers who buy from BCBS and got negative feedback, it reversed the decision and extended the waiving of costs.
Mary MacDonald is a staff writer for the PBN. Contact her at MacDonald@PBN.com. Writer Matthew Enright contributed to this report.












