For decades, Rhode Island’s two largest hospital systems have been rivals, each enduring similar financial pressures on their own in a small but competitive market.
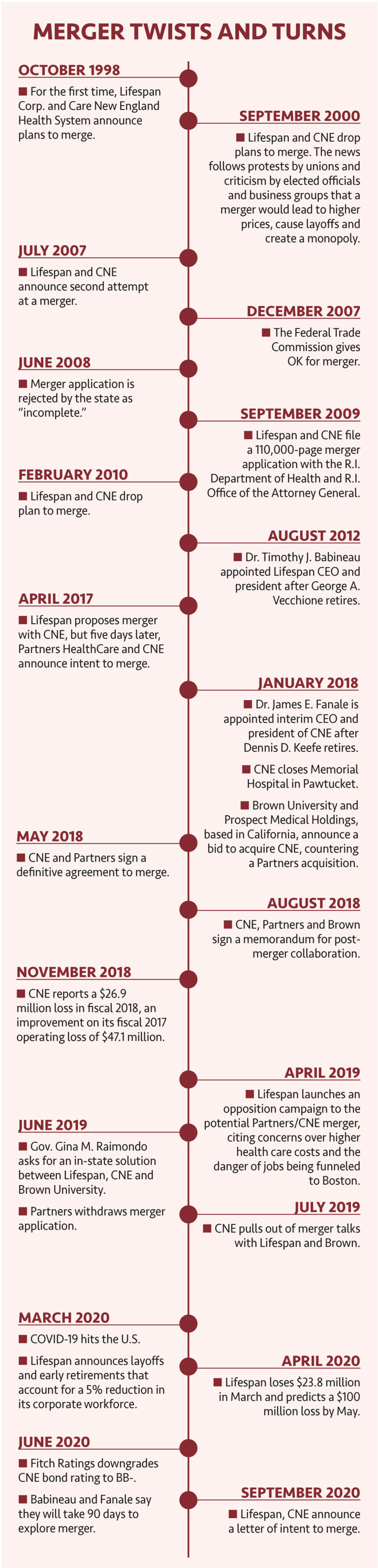
Several attempts over the years by Lifespan Corp. and Care New England Health System to join forces collapsed, including when Gov. Gina M. Raimondo stepped in last year to encourage renewed negotiations between the local entities.
It took a pandemic to finally end the impasse.
After collaborating for months in the fight against COVID-19 – combined with the mounting costs of the public health crisis – the hospital groups have signed a letter of intent to merge and form a unified academic health care system that would also include Brown University.
The announcement on Sept. 9 was touted by top executives at Lifespan and CNE as a win for the two organizations, as well as for Brown and the state because a united local institution would be stronger in an industry marked by upheaval and uncertainty.
But as the merger process moves ahead, questions remain about how such a move will alter the state’s health care landscape.
Observers say that if a merger does come to fruition, job cuts almost certainly will follow. The two systems employ more than 23,600 people at eight hospitals.
And there are worries that combining the dominant players in Rhode Island’s health care sector will dramatically cool off the competitive climate and lead to higher prices for care.
Labor officials also raise concerns about diminishing the quality of care.
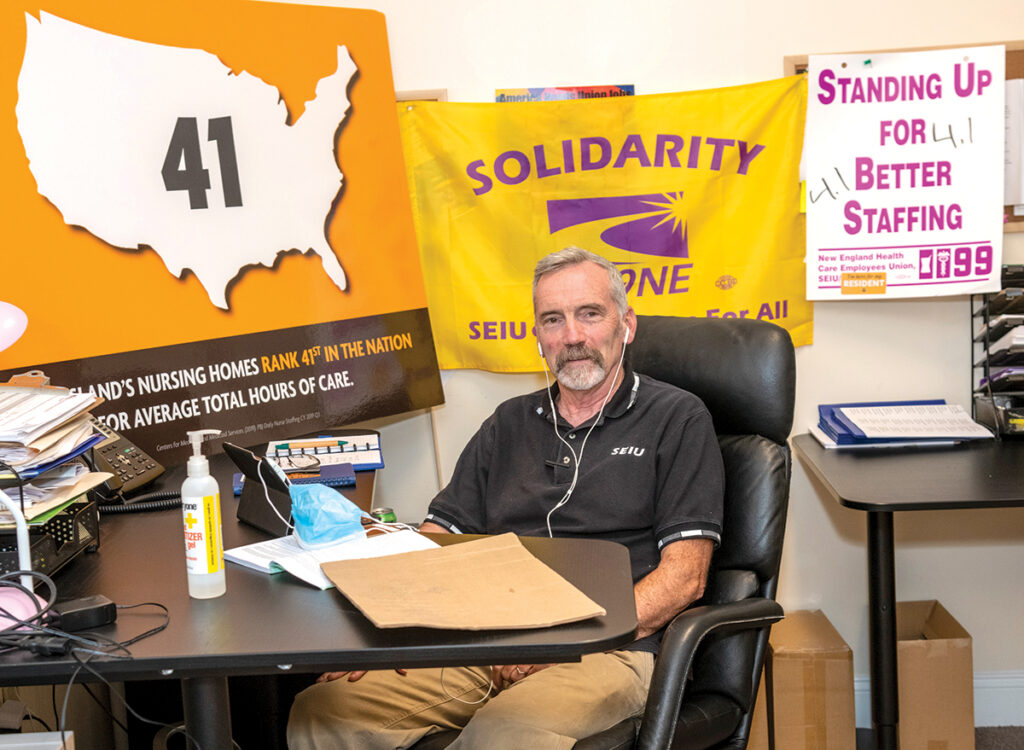
“If we have a merger, does that make us more resilient? Does that improve outcomes of patients? Particularly those from underserved communities,” said Patrick Quinn, executive vice president of Rhode Island for Service Employees International Union District 1199 New England, which represents about 2,300 CNE employees.
“It has got to be outcome-based. It can’t just be, ‘We have to do this because we can’t afford to have two different systems,’ ” Quinn said.
In announcing the plan to merge, hospital executives downplayed those concerns.
“Combining our investment in our physicians, clinical staff, researchers, technology and other health care staff will greatly help us continue to fulfill our mission of providing world-class health care to our patients, advancing medical discoveries and serving as a vital economic engine for our state,” Lifespan CEO and President Dr. Timothy J. Babineau said.
[caption id="attachment_344668" align="aligncenter" width="1024"]
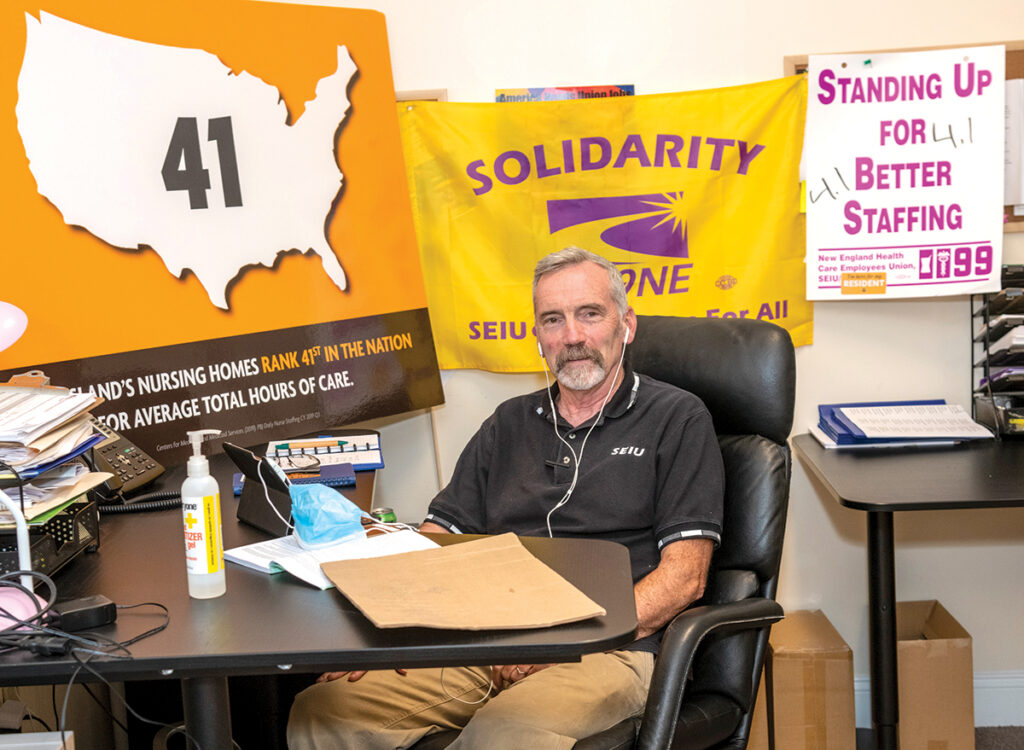
LEERY LABOR: Patrick Quinn, executive vice president of Rhode Island for Service Employees International Union District 1199 New England, which represents about 2,300 Care New England employees, wants a community discussion about the proposed merger. / PBN PHOTO/MICHAEL SALERNO[/caption]
LENGTHY PROCESS
One thing is not in doubt: There’s a lot at stake.
Lifespan operates Rhode Island Hospital, Hasbro Children’s Hospital, The Miriam Hospital, Bradley Hospital and Newport Hospital, while Care New England runs Women & Infants Hospital, Butler Hospital and Kent County Memorial Hospital.
Once the details of the merger agreement are hammered out between Lifespan and CNE, the proposal will face regulatory scrutiny from the R.I. Department of Health and the R.I. Office of Attorney General, as well as from the Federal Trade Commission.
The Department of Health has declined to comment on the potential merger or how it might impact patient care, but spokesman Joseph Wendelken said the review process could last at least several months.
Babineau and Dr. James E. Fanale, CEO and president of Care New England, said once a detailed plan is drawn up, they expect a regulatory review to take at least a year.
While not commenting specifically on a potential Lifespan-CNE merger, Attorney General Peter F. Neronha said he will focus on three health care issues when he reviews the plan – outcome improvements, accessibility and affordability.
“You can deliver quality health care, but if you’re not delivering it to everybody who needs it, you haven’t solved the problem,” Neronha told Providence Business News. “It’s got to be accessible. Rates have got to be affordable.”
Because Lifespan and CNE control a majority of hospital beds in Rhode Island, the proposed merger will likely get a close inspection from the FTC, the agency overseeing antitrust concerns.
Previously, Fanale has said getting past the FTC would present a significant hurdle to complete such a merger. The agency said it does not comment publicly on mergers and acquisitions unless it moves to block a transaction.
Robert Hackey, a professor of health policy and management at Providence College, said a “good” merger and affiliation increases the value of health care by reducing costs, improving outcomes or both, while a “bad” merger helps providers negotiate higher prices and avoid improving outcomes and efficiency.
“If we consolidate specialized services under one roof, then all of the players on the team get more practice and the outcomes tend to improve,” said Hackey, who teaches an annual seminar on health care mergers at PC and Brown. “But when you bring these hospitals together, they have more pricing power. And what they’re going to do is use that pricing power to negotiate higher prices with insurers.”
Hackey said this issue of pricing power is particularly relevant in Rhode Island because this merger would bring more than half of the state’s hospitals under the control of one entity.
Cory King, the policy director at the R.I. Office of the Health Insurance Commissioner, which does not have a say in the hospital merger, said provider consolidation, in general, could result in higher prices, insurance premiums and out-of-pocket medical expenses.
“There’s also a concern that provider consolidation does not improve quality of care, which is important because when you’re paying a premium for an insurance product, which allows you to access services, you want to make sure you’re actually getting something of value in exchange for that,” said King. “If there’s no relationship between increasing consolidation and quality in terms of improving care, then what did you actually get? Particularly if you’re paying a higher price now.”
 LIMPING ALONG
LIMPING ALONG
Lifespan and CNE executives say this is the fourth attempt at a merger for the two systems since the 1990s, but this one is different.
As it stands now, the two organizations are limping through financial troubles separately, a situation exacerbated by the coronavirus.
A restructuring effort by Lifespan before the pandemic led to 55 layoffs, the early retirement of more than 200 and the elimination of 87 positions in corporate services. Still, Lifespan reported a $23.8 million loss for the month of March, which equaled the hospital group’s reported loss for the entire 2019 fiscal year.
Lifespan has, however, received about $130 million so far in pandemic-related federal aid, according to WPRI-TV CBS 12. The station reported Lifespan has benefited disproportionately compared to Care New England because much of that aid has been tied directly to COVID-19 admissions.
Care New England reported an operating loss of $22.8 million in the second quarter.
Before the pandemic, the two hospital systems rarely collaborated. But that changed, as an overwhelming surge of patients sick with COVID-19 seemed imminent. The two groups scrambled to outfit field hospitals with beds, working through staffing issues and making joint decisions on things such as the cancellation of elective surgeries.
The two hospital groups had collaborated on a small scale before, most notably an affiliation between CNE’s Women & Infants and Lifespan’s Hasbro through the Fetal Treatment Program, a cooperative effort to perform in-utero surgeries and other complicated fetal procedures.
But the successful pandemic partnership planted a seed.
“We looked at each other and said, maybe it’s worth one more conversation trying to bring our organizations together,” Babineau said.
After taking 90 days to discuss a consolidation, the boards of directors of each system agreed on Sept. 8 to sign a letter of intent to merge.
That development has answered the hopes of Gov. Gina M. Raimondo, who in June 2019 intervened to get the two sides to the negotiation table when it looked as if Boston-based Partners HealthCare would acquire CNE.
Lifespan had publicly attacked CNE’s deal with Partners HealthCare, and when Raimondo stepped in, Partners – now known as Mass General Brigham – withdrew its bid for CNE. A month later, talks between Lifespan and CNE fell apart, too.
Earlier this month, Fanale said the recent cooperation between the hospital groups during the coronavirus crisis put past disagreements into perspective. “When you start working together, it kind of melts away all the past stuff and [makes you] realize what you could do together,” he said.
Raimondo was updated over the last three months while Lifespan and CNE rekindled discussions, but she didn’t lead the conversation, according to Audrey Lucas, the governor’s spokeswoman. Now Raimondo is “cautiously optimistic” that there will be a Rhode Island-based academic medical center with Brown’s involvement, Lucas said.
Raimondo has long sought an academic medical center controlled by local interests, believing such an arrangement ensures top-notch doctors would remain in Rhode Island, and would drive medical innovation and research locally.
For her part, Brown President Christina H. Paxson said she was “thrilled” that Babineau, Fanale and their respective boards voted to merge, calling a collaboration among the three institutions “the best solution.”
TAKING SHAPE
What would a consolidated entity look like? It’s too early to tell.
On the day that the intent to merge was announced, Fanale told PBN that the executives had not determined who would lead the new system, or even what the name of the organizations would be. The structure of Brown’s involvement hasn’t been defined, and also not decided: how much of the workforce would be reduced to fit the new system, Fanale said.
[caption id="attachment_344664" align="aligncenter" width="1024"]

TEAM EFFORT: Lifespan’s Dr. Francois Luks, left, and Care New England’s Dr. Stephen Carr meet in 2018 with parents Emily and Brian Hess, of Attleboro, as Emily holds her infant son, Selwyn. The doctors had operated on Selwyn in utero as part of the Fetal Treatment Program, a collaborative initiative of CNE and Lifespan. The boy at right is another one of the Hess’ children. / COURTESY LIFESPAN CORP.[/caption]
Hackey noted some potential sticking points as both sides negotiate an agreement.
“We’ve had some personality challenges on who is taking over the leadership role,” said Hackey, referring to media reports last year that CNE – the smaller of the two systems – wanted Fanale installed as leader of a merged entity before talks fell apart in July 2019.
There is a duplication of services that the two hospital groups will have to work through. As it stands now, both systems combined have more facilities and hospital beds than needed in the market, he said.
Hackey pointed to a spat that was touched off in 2017 between Lifespan and CNE when Rhode Island Hospital sought to create an obstetrics unit that would compete with nearby Women & Infants Hospital despite declining births and excess capacity. That unit never became reality.
“Rhode Island has historically had a difficult time coordinating care and imposing order on it,” said Hackey.
At this point, United Nurses and Allied Professionals says it is keeping an open mind about a potential merger.
The union’s Local 5098 represents about 2,700 employees at Rhode Island and Hasbro Children’s hospitals. Local 5008 represents another 1,500 workers at Kent Hospital.
“We welcome the opportunity to meet with both organizations and discuss a path towards developing a new health delivery system … that prioritizes patient care and adequately supports world-class caregivers,” UNAP President Linda McDonald said in a statement. “Our unbending priority will be the preservation of critical health services and jobs that are part of the community and provide care close to home.”
Quinn said he’s not necessarily opposed to a merger, either, but he’s looking for a broad community discussion involving all stakeholders.
Quinn doesn’t believe CNE or Lifespan has provided an answer to whether a merger will help patient outcomes or be beneficial to employees.
“These decisions are too important to be left to just a few individuals,” he said. “However well-intentioned [Babineau and Fanale] may be, it needs to a broad conversation with all aspects of the community invited and engaged.
“When you combine the two, you have one gigantic employer,” he said. “You’re just creating a very powerful employer and provider of services that can engage in all kinds of anti-competitive behavior.”
[caption id="attachment_344666" align="aligncenter" width="1024"]
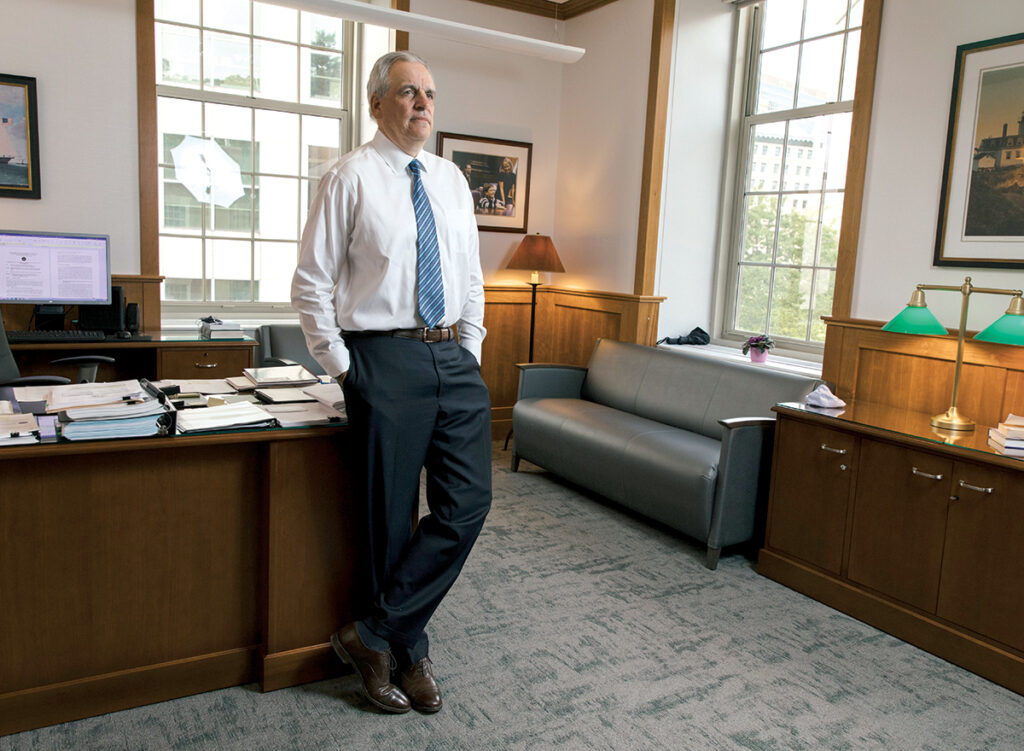
‘You can deliver quality health care, but if
you’re not delivering it to everybody who needs it, you haven’t solved the problem.’
PETER F. NERONHA, R.I. attorney general / PBN PHOTO/RUPERT WHITELEY[/caption]
UNSUSTAINABLE?
In an interview last month – before the decision to pursue a merger – Dr. Raymond Powrie, CNE’s chief of medicine, said he had seen benefits of both competition and collaboration throughout the pandemic.
“I think it’s very important for the people of Rhode Island that our two organizations make a very serious effort to find a way to design an approach to coming together that would both allow collaboration, lower costs and enhance care,” he said. “I think some things are best done through competition and some things are best done through collaboration.”
However, Powrie acknowledged that the further financial strain brought on by the pandemic was felt in day-to-day decisions.
“We’re definitely trying to do less than more and double check what we do spend is on a priority,” said Powrie. “Hard decisions have been made.”
Powrie said care has not been put at risk or compromised because of these financial pressures.
“Do we think this is a sustainable situation? Can we do this for two or three more years like this? No,” said Powrie.
Alexa Gagosz is a PBN staff writer. Contact her at Gagosz@PBN.com.














As a Trustee Emeritus of Women and Infants Hospital, I have long advocated for the formation of a true Academic Medical Center in Rhode Island by the merger of what is now Care New England with the Lifespan system and the Brown Medical school. Having such an entity in our State would stimulate exciting growth in the “Meds and Eds” sector of our economy through research and private start up ventures, while reducing redundancy in many administrative functions and better coordination of individual patients’ care. Indeed it is the only path I see to Rhode Island maintaining control over its own health care system in the long run. Recent forays into the State by Yale to our South, and Boston based Partners/Mass General Brigham with Care New England have exposed the vulnerability of our disjointed acute care network to outside control.
Presently I serve on the Board of South County Health, a very highly acclaimed and demonstrably excellent community hospital system with several standout clinical programs. Many people may not recognize that we are the last remaining independent community hospital in the State. While I can only speak for myself at this point, it seems clear to me that the combined Lifespan/CNE entity will pose a daunting competitive prospect for South County, whose role should really be as a collaborative feeder system rather than a competitor fighting to remain under community control. It has struck me that if our State, which will need to exercise expanded oversight of the new system to control prices in any event, could find a way for the new AMC to divest Kent Hospital to combine with South County under the leadership of the latter (Kent no longer has an independent Board) it might allay some potential regulatory concerns about an in-market system with such market share hegemony as Lifespan/CNE would have, while enhancing the critical mass of patients and administrative efficiency that such entities as South County Health will need to survive in the rapidly consolidating health care environment.
It is just a thought at this point but one I hope may receive some analysis and consideration as this historic health system restructuring continues.