NEW YORK – Health insurers across the United States will race to enroll more seniors in lucrative government-backed Medicare plans this month, even as a roiling debate over the role of private companies in health coverage shapes the presidential race.
The plans, known as Medicare Advantage, are the private-sector, taxpayer-financed alternative to traditional Medicare. Selling them has become a crucial profit center for the insurance industry: Baby Boomers are aging into the program, propelling its growth, while at the same time health insurance products sold to people under 65 are facing pressure from all sides.
The private plans also sit squarely in the middle of the race for the presidency: Some candidates for the Democratic nomination, including Senators Bernie Sanders and Elizabeth Warren, have backed a proposal to do away with private health insurance across all markets. Last week, President Donald Trump signed an executive order aimed at bolstering Medicare Advantage, and said Democrats would upend the program.
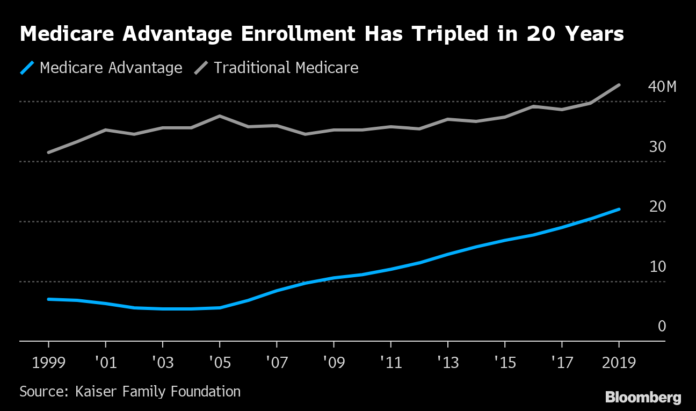
In 2019, about 22 million people, or roughly a third of all Medicare enrollees, got their Medicare coverage through the private plans. For each person who signs up, the insurers collect a fee from the government. It was $11,545 on average this year, which adds up to about $254 billion. The Medicare Advantage enrollment period opens Oct. 15.
Insurers see it as a lucrative market they can’t afford to pass by. Medicare products are the biggest business at the biggest health insurance company, UnitedHealth Group Inc.’s insurance unit. Centene Corp. agreed to pay $15 billion this year for WellCare Health Plans Inc. in part to get access to the company’s large Medicare business. Startups like Clover Health, which has raised more than $900 million from investors including GV, Alphabet Inc.’s venture capital arm, are targeting Medicare customers with new technologies intended to deliver care more efficiently.
UnitedHealthcare will sell Medicare coverage in 100 new counties in 2020, reaching 90% of the eligible market. Humana Inc., which specializes in Medicare Advantage, will expand to 29 new counties. Humana CEO Bruce Broussard told investors in July that membership was growing at the fastest pace in a decade, and the company expects to add half a million members this year. Cigna Corp., which has a comparatively smaller Medicare business, is expanding to 37 new counties next year and projecting 10% to 15% average annual membership growth through 2025. CVS Health Corp.’s Aetna unit is expanding to 264 new counties in 2020.
Anthem’s Medicare Advantage membership grew by 25% in the 12 months ending June 2019, far faster than any other category. Anthem is expanding to 77 new counties in 2020.
Seniors in traditional Medicare can go to any doctor or hospital that participates, as most do. Those who choose Medicare Advantage plans trade that freedom of choice for an insurance company’s more limited network. In exchange, they get extra benefits. Medicare Advantage policies often wrap in prescription-drug plans, vision and dental care. Many offer free gym memberships or fitness programs. They also cap members’ total out-of-pocket costs. In traditional Medicare, seniors have to buy policies known as Medicare supplement or Medigap plans to limit their out-of-pocket expenses.
Starting in 2019, a federal rule change permitted Medicare Advantage plans to offer other perks like transportation and meal delivery. The goal is to address so-called social determinants of health, the many non-medical aspects of people’s lives that affect their well-being. Plans will offer a greater variety of those benefits in 2020.
Some Cigna plans in Texas will pay for air conditioners for the first time next year. Anthem will offer pest-control services, because vermin can affect chronic health conditions such as asthma. Carriers are also testing benefits like adult day care; home safety improvements, like grab bars, to prevent falls; and in-home help for people who need assistance bathing or dressing.
“We actually find a lot of beneficiaries are living in environments that really need support and help,” said Martin Esquivel, vice president of Medicare product management at Anthem.
Medicare doesn’t provide those things in its traditional fee-for-service program, partly because of the risk of inappropriate payments or fraud. In Medicare Advantage, the government’s payment to plans is limited, so that risk is managed by the plans.
The growth of Medicare Advantage shows demand for private managed-care plans exists even when seniors have a purely public option. “No one’s forcing them to do this,” said Dan Mendelson, founder of consultant Avalere Health and a partner at private equity firm Welsh Carson Anderson & Stowe. Seniors are increasingly comfortable giving up some choice of doctors in exchange for Medicare Advantage’s perks, he said. “It’s the choice that makes it really remarkable, that seniors are choosing this.”
While two-thirds of Medicare enrollees choose to stick with the original program, that share is declining. Mendelson said Medicare Advantage enrollment has grown by 8% annually in recent years. At that pace, more than half of Medicare members will be in private plans by 2025, he estimates.
Many people can get Medicare Advantage for no additional premium beyond what they pay for traditional Medicare. The average monthly premium for Medicare Advantage is $23 in 2020, down from $26.87 the prior year, according to the Centers for Medicare and Medicaid Services. It’s at the lowest level since 2007.
Plans have historically been paid generously. A decade ago, Medicare paid private plans 14% more than it would have spent for the same beneficiaries in the traditional program, according to the Medicare Payment Advisory Commission, known as MedPAC, which counsels Congress on Medicare policy. That helped finance additional benefits that enrollees found attractive, but it raised the program’s costs and put little pressure on plans to deliver more efficient care. The 2010 Affordable Care Act lowered those payments. They’re now about 1% above traditional Medicare payments, according to MedPAC.
People who choose to enroll in Medicare Advantage plans also typically have lower health spending before they enroll, compared with similar people in traditional Medicare, according to an analysis by the Kaiser Family Foundation. That means the way payments are set “may systematically overestimate expected costs of Medicare Advantage enrollees,” the Kaiser researchers wrote. Plans have been also faulted by government watchdogs for improperly denying care.
Medicare Advantage plans pay about 86% of their premium revenue out in medical claims, a similar proportion to other health insurance products, according to a separate Kaiser Family Foundation report. But the opportunity to profit is higher. Partly because Medicare beneficiaries use more medical care than younger people, there’s more money at stake for each member. Gross margins in Medicare Advantage – the difference between premiums collected and claims paid, before counting administrative costs – are about $1,600 per enrollee, roughly double the value in commercial plans, according to Kaiser’s analysis.
“This appears to be a fairly profitable market,” said Tricia Neuman, director of the Kaiser Family Foundation’s program on Medicare policy. The group sees more carriers enter the market than exit each year. “If it weren’t profitable, they wouldn’t be doing it,” Neuman said.
Big winners
The market for Medicare Advantage plans has become increasingly concentrated. In 2018, the top four Medicare organizations had 59% of enrollment, up from 46% in 2011, according to MedPAC. And while it may seem like an attractive market, it’s difficult for new competitors to enter.
“We had no idea how hard it would be, how long it would take, the infrastructure we’d have to develop,” said Vivek Garipalli, chief executive officer of Clover Health. The company has about 42,000 members, mostly in New Jersey.
Other new technology-focused insurers are trying to break into the market. Oscar Health announced its first Medicare plans this year. Startup Devoted Health, which is led by former Obama administration officials, raised $360 million to launch its Medicare Advantage plans in 2019.
Those companies are betting that technology can deliver better care more efficiently, by using data to help physicians manage patients with chronic conditions, for example. Medicare Advantage is an ideal proving ground to test that idea, because plans make money if they can deliver savings without compromising quality.
“Health care has effectively had zero productivity gains over the last 20 years,” said Bob Kocher, a partner at venture firm Venrock. The firm backed Devoted Health and Kocher served as the company’s chief medical officer for a year. “There should be a lot of pent-up opportunity here to apply technology to make health care much more productive, and that would also make health care more affordable.”
John Tozzi is a reporter for Bloomberg News.











