Melinda Lemos-Jackson sought hospice care for her mother soon after her Parkinson’s disease was deemed to have reached its end stage last January.
Medicare pays for hospice – specialized end-of-life care focused on physical and emotional comfort, spirituality and support for the family – when a patient has been given less than six months to live and agrees to forgo life-extending treatments. Alice Lemos, 74, qualified.
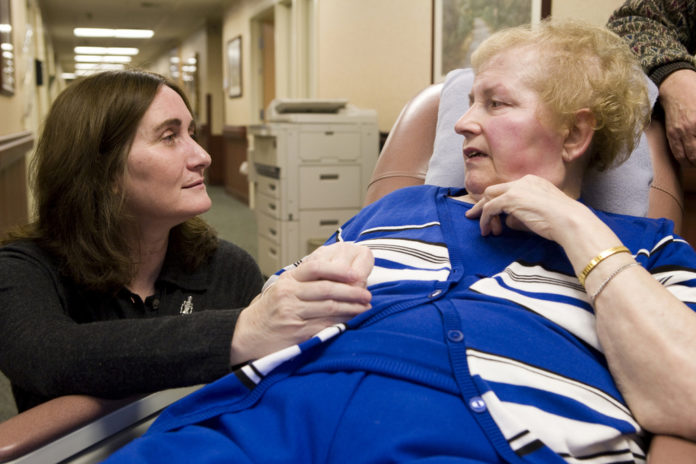
First at home, then at Grandview Center, the Cumberland nursing home where she’s now living, a nurse, a social worker and a certified nursing assistant from Home & Hospice Care of Rhode Island have helped Mrs. Lemos keep pain and discomfort at bay, given her baths, massages and the occasional manicure, and offered emotional support to the whole family.
“It’s been very, very valuable,” Lemos-Jackson said. “These last stages of Parkinson’s are horrible and cruel, and because of the expertise of Home & Hospice Care, they really know how to provide support.”
Alice Lemos was given last rites just before Thanksgiving but has lived longer than doctors predicted. Medicare won’t cut off payments, but if providers like Home & Hospice Care have too many like her – patients who outlive their prognoses – they could face penalties.
Lengths of stay for hospice patients are increasingly under scrutiny nationwide because some hospices – particularly, for-profit institutions in the South and West – have had so many patients exceed the six-month time frame that Medicare has charged them back millions of dollars: $166 million from 220 hospices in 2005, according to the Medicare Payment Advisory Commission.
Since a policy change in 1998, hospices have not been penalized for individuals’ exceeding the six-month limit. Rather, Medicare sets an average per-patient allowance ($21,410 in 2007, or slightly more than five months’ worth at $135 per day). So if a hospice serves 100 patients this year, it’s fine so long as the total it charges to Medicare doesn’t exceed $2,141,000.
For Home & Hospice Care of Rhode Island, where the median length of stay is 13 days, that means the cap is a not a financial concern, said Analee Wulfkuhle, president and CEO.
“Actually, in the last three years, only one hospice in New England has had a cap issue,” she said.
However, the nonprofit agency, which serves about 400 patients at any given time, is still watching the national debate closely. There’s a concern in the industry that with Medicare costs rising rapidly – and hospice coverage costs nearly tripling from 2000 to 2005 to $8.2 billion – Congress might tighten rules in a way that affects all hospices.
A more immediate concern is that patients with terminal but less-predictable diseases, such as Alzheimer’s, will not be referred to hospice for a while out of concern they may not be truly eligible, and thus may be denied valuable end-of-life supports.
“It’s primarily the little old lady that is so fragile, you’re concerned a puff of wind might blow her away – but she might also live on for some time,” Wulfkuhle said. The hospices now facing repayment demands may be taking such patients too soon, when other long-term care options are more appropriate, she said. But for most hospices, especially in this region, the opposite is a greater concern – that people don’t get appropriate, timely end-of-life care.
“In the Northeast, there’s still a sense that hospice is for the final days of life, that you call hospice when you call the priest and the undertaker,” said Dr. Edward M. Martin, medical director for Home & Hospice Care. “It’s really very late in the patient’s illness.”
Patients such as Alice Lemos are the exceptions at the agency; only 5 or 6 percent will ever surpass the six-month mark, Martin said – though at any given time, 20 to 25 percent of the active roster involves patients who have been enrolled for several months.
If, after about four months of services, a patient appears to be getting better, Wulfkuhle said, “we look at what other supports we could offer” outside the hospice setting. However, “we also feel very strongly that if someone goes past that six months, and they still need our services, we’ll keep them on.”
Recent research has shown that hospice care can actually extend life in some cases. Colleen MacTavish-Thurber, the nurse on Alice Lemos’ hospice team, attributes it to the extra level of care, which stabilizes patients and lifts their spirits. John Lemos said he’s seen that not only with his wife, but with another nursing home resident who he’s noticed never wants to eat his meals, but will when the hospice volunteer comes in.
In October, Duke University’s Sanford Institute of Public Policy issued a study showing that hospice also reduces Medicare costs by an average of $2,309 per patient. For cancer patients, Medicare saved money with hospice up to 233 days of care; for non-cancer patients there were savings up to 154 days of care. But despite the higher cost of longer hospice stays, the researchers concluded that “more effort should be put into increasing short stays as opposed to focusing on shortening long ones.”
Overall, hospice use is growing steadily. In 2006, 1.3 million patients received care from 4,500 hospice providers, according to the National Hospice and Palliative Care Organization.
Martin, the Home & Hospice medical director, hopes policymakers remain cognizant of the value of these services and don’t undermine the system. Twelve years ago, Medicare cracked down on lengths of stay, he noted, and the industry – including his agency – has yet to fully recover. “I think the big concern is that federal agencies will get the message that they need to tighten up on this [again],” he said. •












